BSC and IrsiCaixa create bioinformatics method to predict the effectiveness of drugs with HIV mutations
The effectiveness of antiretroviral drugs used to treat HIV (human immunodeficiency virus) is frequently affected by the virus’ ability to develop genetic mutations.
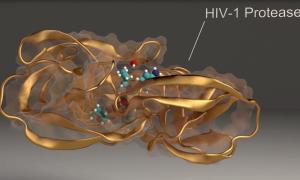
Barcelona Supercomputing Center (BSC) and IrsiCaixa, the Catalan AIDS Research Institute, have developed a bioinformatics method to predict the effect of each mutation on the resistance of the virus to such drugs. An article published in the Journal of Chemical Information and Modeling explains how this method has effectively predicted the resistance of the virus with genetic mutations in the HIV-1 protease, a protein which is essential for the replication of the virus, to the drugs amprenavir and darunavir. The method could easily be applied to other drugs and proteins.
Currently, information obtained from other patients is used to predict the effects of HIV mutations on drug effectiveness. Built cumulatively through clinical experience, this knowledge is useful but has limitations. For example, it is unable to provide answers when the virus develops a mutation which hasn’t previously been recorded. The method created by BSC and IrsiCaixa overcomes these drawbacks by providing predictions based on the characteristics of each genetic mutation and on the changes which the mutation produces in the virus’ proteins which act as targets for the drugs.
The BSC-IrsiCaixa method combines HIV DNA sequencing, identification of genetic mutations, computational protein modelling and the simulation of drugs binding with the proteins of the virus. The entire bioinformatics analysis can be performed in fewer than 24 hours on relatively small-scale computing equipment available to any laboratory. One of the main features of the system is the use of PELE, a piece of software developed at BSC to predict how drugs will interact with their targets, which has been shown to have competitive advantages over commercially available software.
Web access
BSC has created an automatic platform, available for free via the web, on which researchers can enter a patient’s HIV-1 PR protease genomic sequence and predict the effectiveness of prescribing the drugs amprenavir and darunavir. For the moment, these are the only predictions available, pending advances in research on the effect of HIV mutations on other proteins within the virus and interactions with other antiretroviral drugs.
An example of the personalised medicine of the future.
BSC researcher Victor Guallar, who appears as principal investigator in the article published today in the Journal of Chemical Information and Modeling and is the lead developer of PELE, explains that ‘this system is one of the first tangible steps in the area of what will eventually be personalised medicine, where treatment will be decided following genetic analysis of the causes of the disease in each patient and of which drug would be most effective in each individual case’.
‘In this study we demonstrate how to connect routine clinical diagnosis of HIV-1 with structural computer modelling. This is a multidisciplinary proof of concept which overcomes the limitations of current practice when deciding antiretroviral treatment and which, in addition, allows new drugs to be designed more quickly,’ adds IrsiCaixa researcher Marc Noguera-Julian, who participated in the study.
Vídeo of one of the simulations.